Faculty Expertise
Our faculty members are nationally and internationally known for their expertise in medical imaging, interventional radiology, diagnostic medical physics, and nuclear medicine
Education Programs
We offer comprehensive radiology residency programs and subspecialty fellowship programs
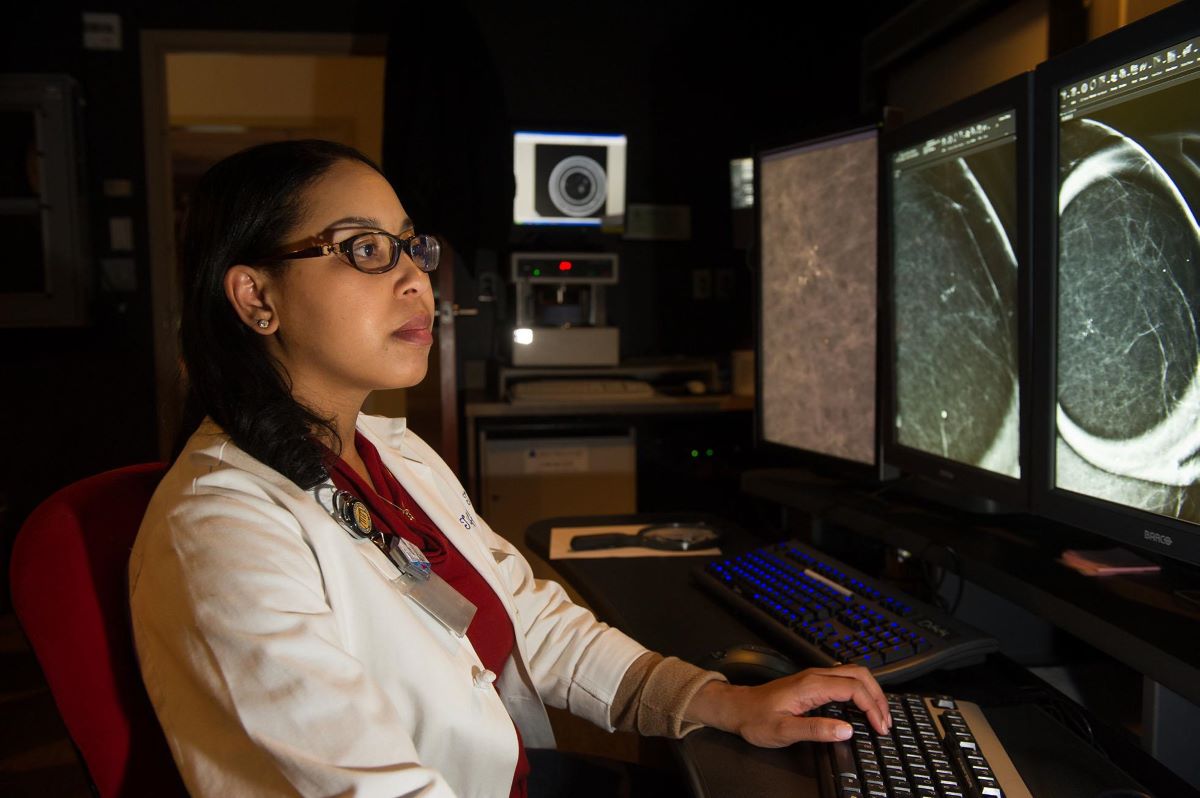
Research
VCU Department of Radiology faculty and full-time research scientists uphold the tradition of innovative discoveries and excellence in research.
Our research portfolio extends from basic activities to clinical trials, including:
- Breast shielding for CT (computed tomography) radiation protection
- Magnetic resonance cholangiopancreatography (MRCP) in biliary and pancreatic imaging
- Virtual colonography
- Application of CT in trauma
VCU Health Radiology at Stony Point Earns ACR Prostate Cancer MRI Center Designation
A First in Virginia, VCU Health Radiology at Stony Point Receives Elite Distinction for Safe and Effective Diagnostic Care for Individuals at the Highest Risk for Prostate Cancer.
 Richmond, VA - April 2024 - VCU Health Radiology at Stony Point has been designated a Prostate Cancer MRI Center by the American College of Radiology® (ACR®).
Richmond, VA - April 2024 - VCU Health Radiology at Stony Point has been designated a Prostate Cancer MRI Center by the American College of Radiology® (ACR®).
The ACR Prostate Cancer MRI Center designation is a voluntary program that recognizes facilities that commit to practice safe, effective diagnostic care for individuals at the highest risk for prostate cancer.
In order to receive this elite distinction, facilities must be accredited by the ACR in the body module, as well as undergo a rigorous assessment of its MRI imaging protocol and infrastructure.
VCU Health is the only health system to achieve the accreditation in Virginia and one of only 65 medical facilities in the United States.
The ACR, founded in 1924, is one of the largest and most influential medical associations in the United States. The ACR devotes its resources to make imaging and radiation therapy safe, effective and accessible to those who need it. Its 36,000 members include radiologists, radiation oncologists, medical physicists, interventional radiologists and nuclear medicine physicians.
For more information about the Prostate Cancer MRI Center designation, visit: https://www.acraccreditation.org/Prostate-Cancer-MRI-Center
2023 Impact Report
Image of Excellence in Action
VCU Department of Radiology 2023 Impact Report explores our contributions to VCU Health and our accomplishments in the field of radiology. Read our VCU Radiology 2023 Impact Report [PDF].
New VCU Pediatric Radiology fellowship program
Our one-year ACGME accredited Pediatric Radiology fellowship affiliated with the Children’s Hospital of Richmond at VCU integrates clinical excellence with research and teaching in all aspects of pediatric radiology.
Learn more about our Pediatric Radiology fellowship